Network Spotlight
The network aims to collaborate with the broader scientific community through conducting clinical studies, publications, conference presentations and sharing data in a central repository (DASH). We want to maximize the value of the data these women graciously provide to us to learn more and find the best treatments.
NICHD
Meet the members of Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD)!
Donna Mazloomdoost, MD, FACOG, Project Scientist, joined the Pelvic Floor Disorders Network (PFDN) in February 2017. She completed her training in OBGYN and practiced as a general OBGYN at Georgetown for 6 years. During that time, as she developed long-term relationships with her patients, she encountered more pelvic floor conditions than she had ever been aware existed. As a result of this, she went back to pursue a fellowship in urogynecology. By luck, a position in the Gynecologic Health and Disease Branch (GHDB) at NICHD opened as she was moving back to the DC area, and she was contacted by the branch chief at the time about her potential interest in taking the position. Dr. Mazloomdoost considers this one of the luckiest and best career moves she has ever made!

Dr. Mazloomdoost considers having the opportunity to get to know the PFDN investigators and coordinators as the most rewarding and interesting part of working with the PFDN. They are an intimidating group of scientists with regards to their expertise, but you will never meet a kinder, more generous group of physicians and nurses/coordinators. She learned more in the first year from them than she did in her previous years as a physician and will be forever grateful for their mentorship and welcoming nature.
When asked about what impact she envisions in the next 10 years as a result of the PFDN she says, as a subspecialty, very little was known about pelvic floor disorders prior to the establishment of the PFDN. In the past 20 years, the growth and knowledge of this field has been exponential. She believes this network has the potential to decipher the etiology behind these conditions and develop novel/successful therapeutics.

Abisola (Abi) Tepede, PharmD, RPh, MS, PMP, Program Officer at NICHD Pelvic Floor Disorders Network and NICHD Office of Clinical Research. She has served in this role for 3 years.
Dr. Tepede completed her Doctor of Pharmacy Degree from the University of Illinois at Chicago. She followed with a post-PharmD residency and fellowship with Novartis Pharmaceuticals and Massachusetts College of Pharmacy and Health Sciences (MCPHS) University in Boston, Massachusetts. Her work with the NICHD's Division of Extramural Research showcases her dedication to advancing women's and children's health through strategic programmatic activities and resource allocation.
With a determination to translate her clinical research knowledge to low-and-middle-income countries, Dr. Tepede successfully completed a detail assignment with the US Department of State, Embassy Science Fellows Program. Her contributions included enhancing research proposals and building clinical trial infrastructure in Mauritania. She implemented a first-of-its-kind STEM laboratory for pre-university/university students and facilitated collaborations between US research investigators and the Mauritanian research investigators along with their Ministry of Health.


PFDN research is pivotal in executing complex research studies that could change clinical practice guidelines and raise awareness of the condition of pelvic floor disorders to both patients and other medical professionals. She is passionate about helping and serving patients and the ability to collaborate with a group of dedicated and brilliant PDFN researchers has been the most rewarding part. Dr. Tepede values the PFDN’s emphasis on mentorship and paying it forward for the next group of scientists.
Dr. Tepede envisions that the PFDN will continue to assist the patient population of women with urinary and fecal incontinence and pelvic organ prolapse to improve their quality of life. The PFDN is already making strides through current studies with a focus on decentralized clinical trials and public-private partnerships. This could expand to pragmatic clinical trial designs and primary care and/or rural settings.
Previous Spotlights
Meet some of the team at Brown/Women & Infants Hospital!
At Brown/WIH (Women & Infants Hospital of Rhode Island) we have been proud members of the Pelvic Floor Disorder Network (PFDN) since 2011. Our site has grown and changed over the years, and we are happy to feature 3 very important members of our team.
Sarashwathy (Sara) Veera, BS is our Senior Research Assistant and has been involved in numerous PFDN trials including NOTABLe, SUPeR/eSUPeR, ASPIRe/eASPIRe, and MUSA/PROMISe. In addition to recruiting, tracking, and knowing our research participants, she also oversees our IRB submissions.
Leah McKay, BS, MS is a Research Assistant on our team. For PFDN, she conducts follow-up visits and data entry for our eSUPeR, eASPIRe and MUSA participants. She is a quick study and has a knack for developing great relationships with our research participants and making them feel at ease. We look forward to her involvement in our upcoming PFDN trials.
Julia Shinnick, MD became a faculty member in our division this past summer. We had the privilege of working with Julia on many research projects when she was a Fellow on our team. Her knowledge and attention to detail is so appreciated and we look forward to many years of her involvement in the PFDN.

Leah McKay
Leah started with us one year ago and has done a wonderful job focusing on eSUPeR, eASPIRe, and MUSA follow-up within PFDN.
Leah obtained her BA from Penn State. Following graduation, she traveled and lived in Ohio, Texas, and Alaska. Pursuit of her MA in Biology brought her to New England, specifically Massachusetts. After graduation, she worked in a job that didn’t suit her research interests. Urogynecology appealed to her because a family member was having pelvic floor issues and had been treated at one of our fellow PFDN sites!
Leah feels fortunate to work directly with patients in her role within PFDN. Many patients say their experiences are life changing. Leah appreciates how women are constantly learning about their issues and most are satisfied and happy. They know they are in good hands.
When thinking about the PFDN in the next 10 years, Leah anticipates we will continue creating awareness/acceptance and de-stigmatize women’s experiences.
Leah really enjoys science/research. She feels the need to be in a setting where she continues to learn and grow so she can push the boundaries of her current knowledge.
In her spare time Leah participates in indoor rock climbing, which she highly recommends to anyone who might be thinking about it. She is very active and spends time working out at the gym, hiking, and enjoying nature. Leah’s best friend is a 100-pound Doberman named Drax who she describes as the “sweetest boy”. He keeps Leah on her toes!
Meet Smudge – our dinosaur mascot. He has been with the division for several months now and does wonderful work.
Julia Shinnick
Julia Shinnick is a Urogynecologist at Brown/Women & Infants Hospital. After graduating from Emory University School of Medicine in Atlanta, Georgia, she came to Brown for her Ob/Gyn residency training in 2016. She stayed at Brown for Urogynecology fellowship in 2020 and joined as faculty in 2023.
Dr. Shinnick has interests in clinical research. She was initially inspired to pursue a career in Urogynecology through a summer clinical research internship as an undergraduate.
The most rewarding part of working with the PFDN is being able to contribute to studies that help shape the care for patients across the country.
In the coming years, Julia believes the PFDN will have a positive impact through centering patients in the ways that we ask and answer questions.


Sarashwathy “Sara” Veera
Sara started with us as a Student Intern in May,2018. She decided to join our team as a Research Assistant the following year and has since been promoted to Senior Research Assistant.
Sara came to us as a pre-med undergrad looking for clinical work opportunities. She was drawn to areas of medicine that are stigmatized and unique. Sara had a friend who connected her to us. She feels there is an opportunity here for community related health and outreach which is exciting to Sara as this movement in its developmental stages. Sara appreciates how close our research team is with the rest of our department and that we are not alone in our journey.
The most rewarding part of working with the PFDN for Sara is the protocol development process. It is never a “one size fits all” and Sara appreciates the collaboration where we address local issues specific to each site. “It is cool to get perspective all across America”.
When thinking about PFDN in the next 10 years, Sara envisions breaking away from the standard. An example would be the creation of new validated questionnaires and using better informed data collection methods using input from community members.
Sara started out as pre-med but as she has had more exposure, she may re-direct. She is curious about public health and may focus on more experiential learning. Her future position may not fit a template.
In her spare time, Sara is busy! She does a lot of volunteering, is involved with community networks within the area, teaches kizomba and tarraxo dancing, is learning how to forage for mushrooms, crochets, paints, and is a birder. Sara is also a great cook, focusing on South Indian dishes to get in touch with her culture.
Meet some of the team at Kaiser Permanente San Diego!

Kaiser Permanente San Diego has been a member of the Pelvic Floor Disorders Network (PFDN) since 2005. Throughout the years we’ve had the privilege of working with an amazing and talented group of investigators and have had the opportunity of contributing to innovative trials’ growth and success. Kaiser Permanente’s goal has been to improve and provide effective health care to women with pelvic floor disorders.
Gisselle Zazueta-Damian, RA IV, is our Senior Research Associate and Project Manager, who has been a dedicated teammate and has supervised numerous PFDN trials including ABC, ESTEEM, CAPABLe, NOTABLe, SUPeR/eSUPeR, ASPIRe/eASPIRe, and MUSA/PRoMISe. In addition to her supervision in our trials, she is also our lead regulatory personnel for IRB communication and protocol submissions.
Linda Mackinnon, MPH, RA II, is our Lead Research Associate and has been part of our team for 13 years. Linda has also been involved with numerous PFDN trials and she currently directs our eSUPeR, eASPIRe and MUSA trials. Linda takes pride in her work and continues to ensure that our team carries out our PFDN study commitments.

OUT WITH THE OLD AND IN WITH THE NEW

Diana Banales, RA IV, recently relocated to our department to assist with our growing portfolio. She started in the fall of 2023 and has already made a huge impact at our clinic. Diana started her clinical research experience 6 years ago in the Rheumatology Department as an unblinded pharmacist. This is where she was exposed to clinical trials. Diana found them intriguing, which in turn lead to the beginning of her research career. Diana has been a Project Manager for multiple clinical trials within Kaiser Permanente, which include trials with Gastroenterology, Endocrinology, Cardiovascular and Infectious Diseases (COVID-19).
Diana considers herself a newbie to PFDN but has already taken the initiative of leading one of the networks upcoming trials, TULIP. Not being exposed to pelvic floor disorders prior to joining our team, she finds it fascinating learning about pelvic floor disorders and listening to all the ongoing studies, but most of all looks forward to contributing to new and upcoming studies.
Diana is amazed on how all investigators within the network work so closely and diligently to develop new clinical trials. She expects the contributions made by all involved to be successful, impacting women substantially, and envisions herself being part of PFDN for many years to come.
In her spare time, Diana loves to travel and enjoy the beach. Some of her favorite vacationing locations are the Caribbean Islands. Her most recent vacationing island, Jamaica! One Love!!
Vanessa DeLoera, RA II, also recently joined our department to assist with our growing portfolio this past fall. Vanessa began her career as a Medical Assistant and then furthered her education to obtain her phlebotomy license. She was provided the opportunity to join Kaiser’s Department of Research and Evaluation and assisted on a multi-center study for the Epidemiology Department and soon thereafter transitioned to Clinical Trials. This March will mark 10 years since she began her journey in Clinical Trials at Kaiser Permanente San Diego.
Vanessa has been exposed to a vast number of clinical trials - from OBGYN, Gastroenterology, Infectious Diseases, Endocrinology, Cardiovascular, and now Urogynecology. Her experience has motivated her to continue her education and thus she will be starting a vocational nursing program this spring. She is eager to begin contributing in the PFDN and finds it rewarding to be able to work beside a talented group of investigators.
Vanessa’s life revolves around her family – husband, two teenage children, and two small but mighty yorkies, Jordi and Lola. In her spare time, she enjoys hiking and dancing. She particularly enjoys dancing bachata and takes dance classes in various SD downtown venues. Oh La La!!

In addition to our Division Director, Shawn Menefee, our division includes numerous other co-investigators that drive our recruitment including Drs. Gouri Diwadkar, Jasmine Tan-Kim, Kimberly Ferrante, Quinn Lippman, & Tatiana Catanzarite and APP's Christine Doan, Lisa Mager, and Gloria Haley. We would like to highlight our new addition:

Heidi W. Brown, MD, became a member of our Urogynecology division and a scientist of dissemination and implementation for our Department of Research and Evaluation this past summer. As a former Fellow of our team, she has already contributed to many trials within the department.
Dr. Brown’s research focuses on improving access to effective solutions for pelvic floor disorders such as bladder and bowel incontinence and pelvic organ prolapse. She uses community engagement, user-centered design, and iterative testing to inform development, adaptation, implementation, and maintenance of interventions that improve quality of life.
Dr. Brown’s primary research focuses on how to support women to adopt these behavior changes and pursue additional treatments when necessary. She is also interested in developing and testing streamlined implementation strategies to build and maintain productive connections between primary care, specialty care, and community resources.
In her spare time, Dr. Brown enjoys spending time with her husband and 3 sons, dancing, hiking, music, and the beach! Surf's up!
Meet some of the team at Duke University Hospital!

Duke University Hospital has had the privilege of being part of the Pelvic Floor Disorders Network since 2007. We have led several prominent studies within the network with an incredible group of passionate and talented investigators, providers, researchers, and staff. We are so excited to contribute to the innovative and groundbreaking clinical trials that can only be accomplished by the kind of collaboration allowed by multisite network studies!
Dr. Anthony Visco is our Division Chief for Urogynecology and Reconstructive Pelvic Surgery. He received his MD from State University of New York Upstate Medical University and completed his residency in OB/Gyn at the University of Rochester. One of the longest standing members of the PFDN, he has been a clinical site PI of the network for 21 years. His involvement in the PFDN since 2001, just out of fellowship, has been one of the most influential academic experiences of his career. He fondly recalls his first meeting, sitting around the table surrounded by “giants” in the field. Their mentorship about recruitment, trial design, and research techniques laid the foundation for his own contributions. With their encouragement, he was able to confidently challenge conventional practice and the status quo.
During one Steering Committee meeting in his early days, there was a lively discussion regarding whether Botox bladder injections should be reserved for refractory overactive bladder or whether drug naïve patients should be included in a randomized trial they were designing. By respectfully challenging “conventional wisdom”, while also balancing patient safety and autonomy, they were able to design a bold and meaningful randomized trial.
Dr. Visco says the most rewarding part of his involvement in the PFDN is completing studies that many people thought were too difficult or even impossible to accomplish. He feels fortunate to have contributed to the design and recruitment of so many landmark studies in the field and worked with such amazing partners at Duke for more than two decades, including surgeons, research coordinators, and most importantly, the committed patients and research participants. He considers his PFDN partners to be both colleagues and friends.
Dr. Visco remains excited about the future of the PFDN and its positive impact on women’s health. The PFDN’s commitment to innovative clinical and translational research ensures that women’s health continues to benefit from evidence-based advancements. His continued involvement in the PFDN continues to inspire him.
Stephanie Yu is our lead Clinical Research Coordinator for the PFDN. She joined Duke in 2022 and manages eSUPeR, eASPIRe, and MUSA for the site. She is a competitive powerlifter and Brazilian jiu jitsu practitioner who became interested in urogynecology due to the prevalence of pelvic floor disorders among female strength athletes. She is excited to be a part of the network and hopes to contribute to positive advances in women’s health.
Here’s what some of our patients have had to say about being part of PFDN studies
“I chose to participate in [the ASPIRe study] because I want my daughters to be able to have the best possible care if they ever need this kind of surgery.”
“Everyone at Duke has been so wonderful. It makes me happy to help out!”
“I feel proud to get to be a part of medical research. I really hope doing this will help other women.”
“[My surgeon] is the kindest and most caring doctor I’ve ever had. She makes me feel like I’m her most important patient. I didn’t think there were many doctors like that, but when I come in for research visits with a different provider, it turns out all the providers [at Duke Urogynecology] are like that. It feels like everyone truly cares.”
“[Research coordinator] went out of her way to answer all of my questions and send me updates about results whenever I ask for them. It’s exciting to have something to look forward to and be able to say I was a part of this!”
“I like being part of research because I get to have free checkups. [Provider] always takes time to address all of my problems when I’m here.”
“I have never had anyone care about me as much as [masked provider]. Even though I live far away, I chose to stay in [the ASPIRe study] because of how amazing she has been.”
“When [surgeon] asked me about coming in for [SUPeR], I can’t believe he remembered so many details about me. His bedside manner can’t be compared, and he makes me so comfortable when I’m nervous about being in the hospital.”
Dr. Nazema Siddiqui came to Duke in 2007, which is the same year Duke became a site within the PFDN. Her training and clinical practice have been enormously influenced by the PFDN. PFDN trials have always been the way that we test new surgeries, new treatments, and new innovations for women, while also ensuring that our patients are safely cared for under close monitoring.
Her first direct involvement in the PFDN was in 2008 through a writing group led by Dr. Linda Brubaker. She was the most junior person in this group and was quite intimidated! Yet, Dr. Brubaker and others were interested in whatever promoted the best science, and she soon found her voice. In 2022 she was thrilled to step into the role of site PI and continue the tradition of Duke’s involvement with the PFDN and commitment to high-quality clinical trials.
At many levels, we see that conditions that affect women are not prioritized in large-scale research. Yet, the PFDN has been one of the few bright spots and has shown us successful ways to do large-scale, impactful work that helps the lives of women. Over the last two decades PFDN studies have helped us optimize pelvic surgeries, understand the role of physical therapy, and learn more about how the microbiome may be implicated in pelvic health disorders.
Today, Dr. Siddiqui serves as Duke Urogynecology’s Associate Professor and Director of Research, Division of Urogynecology and Reconstructive Pelvic Surgery. She looks forward to expanding the reach into new scientific areas, broader populations of women, and cultivating the next group of surgeon-scientists who will carry the torch and conduct innovative research that helps the lives of women.

Meet some of the team at the University of Chicago!
The University of Chicago is the newest addition to the PFDN but has deep roots to the PFDN. Dr. Kimberly Kenton has participated in the PFDN from its inception in 2001 to 2011. During her tenure with the PFDN she published high impact research which has transformed the Urogynecology landscape, most notably “A Midurethral Sling to Reduce Incontinence after Vaginal Prolapse Repair.” She is thrilled to re-join the network along with her alternate PI Dr. Maggie Mueller, and co-investigators Drs. Christina Lewicky-Gaupp, Sarah Collins, Juro Letko, and Sandy Valaitis. This research powerhouse has diverse research expertise and interest in shared decision making, birth trauma and recovery, genitourinary microbiome, and postoperative activity. In 2024, Dr. Jamie Griffith, a longtime collaborator, joined the team, further diversifying the team’s research portfolio with his expertise in psychometric analysis and patient reported outcome measure development. The team’s diversity in research expertise and interest is paralleled by their diversity in interests outside of work! Our team members enjoy watersports, winter sports, tennis, boating, lake life, rock concerts, biking, hiking, cooking and wrangling the 11 kids and 5 fur-babies they are raising- just to name a few!

Meet our newest team members!

Dr. Jamie Griffith is a professor in the Department of Ob-Gyn at the University of Chicago with a joint appointment in the Department of Psychiatry. He is a clinical psychologist with interests in clinical assessment, behavioral interventions, and clinical decision-making. He is a member of several research teams with a focus on pelvic health. He gave the keynote address to the PFDN in 2023 entitled “Perspectives on patient-reported outcomes”. He works closely with the urogynecologists at the University of Chicago to lend a holistic perspective to both research and clinical care.
Dr. Griffith’s research includes the relationship between cognition and emotion, autobiographical memory, and mental health comorbidities. More recently, he has grown his research to include the intersection of medicine and mental health in areas including chronic pelvic pain and pelvic floor disorders. A common thread of this work is enhancing clinical assessment, making it more efficient for clinicians and patients. For example, one of his R01s funded by NIDDK is focused on connecting patient-reported outcome data to clinical decision-making. Dr. Griffith is leading several projects examining the intersection between mental health and urogynecology, focusing on pelvic floor disorders, addressing disparities in urinary control symptoms, and developing new self-management interventions for women with pelvic floor disorders.

Tara Samsel is one of our Clinical Research Coordinators for the PFDN. She joined University of Chicago last June when she moved to Chicago. She is an aspiring OBGYN and became interested in Urogynecology after conducting her undergraduate research focused on physiological and microbiome changes in postmenopausal and postpartum women. As a new member of the PFDN, she is excited to be involved in the upcoming BASIS and TULIP PFDN studies.
Tara grew up near St. Paul, Minnesota and finished her bachelor’s degree in Cellular & Molecular Biology at Barnard College of Columbia University. While at Barnard, she worked as a research assistant at Columbia University’s Medical Center and Fertility Clinic. She worked in their embryology lab conducting an independent research project adapting a robotics platform to function as an automated liquid handling system for IVF plating. She also earned her Emergency Medical Technician certification while in her junior year. Prior to starting her career at the University of Chicago she interned for two digital women’s healthcare start-ups, Caraway and Allara, developing her interest in gynecological healthcare.

Rowena Jinxuan Shi serves as our Lead Clinical Research Coordinator at the University of Chicago for the Pelvic Floor Disorder Network (PFDN). With just over a year of dedicated involvement, Rowena has embraced her position, aligning herself closely with the network's mission to elevate understanding, treatment, and support for individuals contending with pelvic floor disorders.
Her journey into the realm of pelvic floor disorders began with a passion for research and a deep-seated desire to make a tangible impact in women’s healthcare. After completing her master's degree at the University of Chicago, Rowena naturally gravitated towards opportunities where she could merge her scientific knowledge with genuine empathy for those confronting health challenges. Joining Dr. Kenton’s team and the PFDN provided her with the perfect platform to apply her skills in a field where innovation and empathy intersect. Looking ahead over the next decade, Rowena envisions the PFDN continuing its trajectory of advancement. As she embarks on this journey, she is optimistic that collective efforts will pave the way for a future where pelvic floor health is understood and accessible to all.
In her free time, Rowena loves to travel. Exploring new places allows her to immerse herself in different cultures, try delicious local foods, and marvel at stunning landscapes and architecture. Each trip brings unforgettable experiences and connections, adding colorful chapters to her life story.
Meet some of the team at the University of California at San Diego!

UC San Diego has been a member of the Pelvic Floor Disorders Network (PFDN) since 2006. The Division of Urogynecology and Reconstructive Pelvic Surgery at UCSD seeks to be an international leader in clinical care, research, and education. Our division members are committed to our mission and actively participate in basic science research, clinical outcomes research evaluating interventions for pelvic floor dysfunction, and bladder health promotion. We consider it an honor and a privilege to work with top investigators in the field who are collectively improving healthcare for women everywhere.
Laura Aughinbaugh DNP, WHNP, CNM has been with PFDN as a co-investigator for 8 years! She currently is involved with ESTEEM, ROSETTA, NOTABLE, ASPIRe, E-SUPeR, MUSA, and TULIP.
Laura is a Women's Health Nurse Practitioner and a Certified Nurse Midwife at UC San Diego Health. She has cared for women and for the childbearing family in these roles for 19 years. She currently spends her clinical time serving women in Urogynecology at UC San Diego Health. Laura’s introduction to PFDN started when she joined the UC San Diego Health team of healthcare providers and researchers. The most rewarding part of her participation in PFDN is knowing that the care and healing she offers women within the clinic, can go beyond her day-to-day encounters. She loves that her efforts today, will help improve the lives of women for future generations. There are only so many hours in a day and only so much she can do with her own two hands - PFDN enables her to reach more women through thoughtful investigation and evaluation. Laura is very grateful for the efforts of the PFDN.


Dr. Cecile Ferrando recently joined UCSD, taking over as Fellowship & Research Director of the Urogynecology & Reconstructive Pelvic Surgery Division and Co-Director of the URPS Clinic. While new to UCSD, Dr. Ferrando has been part of the PFDN for many years, having worked as an investigator during her FPMRS fellowship and subsequent faculty position at Cleveland Clinic since 2015. One of her biggest passions is graduate medical and surgical education. In Cleveland, she served as the Program Director of two fellowships and was the Vice Chair of Education for the Department of OBGYN. As a scientific investigator she has published over 100 original research papers. Her research interests include clinical outcomes of pelvic reconstructive surgery. She brings a unique skillset to UCSD and is excited to be an active contributor to their research program, as well as the PFDN.
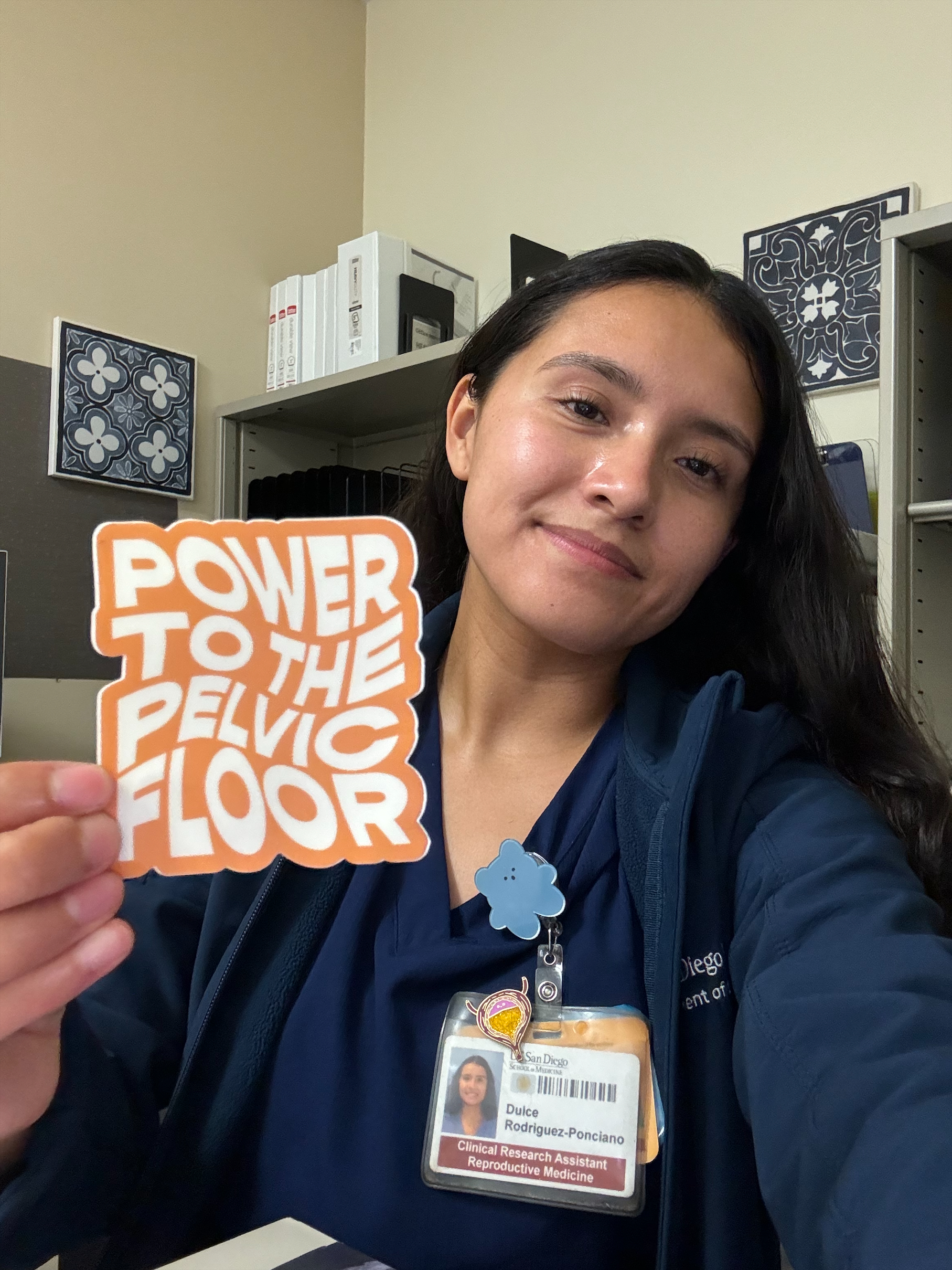
Dulce Rodriguez-Ponciano is one of our Clinical Research Coordinators and has been part of our team for 7 years. She started with us as a Research Assistant in 2017 while completing her undergraduate degree. She has been involved with numerous PFDN trials and currently manages eSUPeR and eASPIRe. Dulce says the most rewarding part of working with the PFDN is establishing meaningful connections with participants and making them feel supported and truly valued.
Dulce grew up in Tijuana, México and currently resides in San Diego. She is passionate about contributing to services that benefit marginalized populations. She has volunteered with various health organizations since 2017. In her free time, Dulce enjoys roller skating and spending time at the beach.
Joseline Sanchez is a Clinical Research Coordinator who started with PFDN back in November 2023.
Right before graduating with her B.A in Public Health from UC Berkeley, Joseline began her clinical research journey at UCSF within the Division of General Pediatrics and Health Policy Studies. Born and raised in San Diego, California, Joseline knew she wanted to return home and continue her passion for Public Health and Medicine, assisting the community she grew up in. It was then that she found herself at UCSD Health.
Her interest in Women’s Health peaked while she assisted in Cervical Cancer research. She appreciates being part of research focused on improving women's health and is passionate about diversifying medical research. She enjoys engaging with women in both English and Spanish and being able to facilitate recruitment efforts.
In her free time Joseline loves to go to the beach, try new cuisines and is always on the hunt for a new Boba spot.
(Pictured above, left to right) Drs. Maria Florian-Rodriguez, David (“Ike”) Rahn, Joseph Schaffer, Clifford Wai, Sunil Balgobin
(not pictured: Dr. Marlene Corton)

UT Southwestern first became a member clinical site in the Pelvic Floor Disorders Network (PFDN) in 2006 (Cycle II) with Dr. Joe Schaffer as the site’s Principal Investigator (PI). We were proud to champion early translational and basic science studies from the Network by developing a biorepository for specimens and tissues collected during clinical trials. UT Southwestern remained the Network’s main Biorepository through Cycle III. In Cycles IV and V, Dr. David (“Ike”) Rahn has been the PI for the site, and Dr. Maria Florian-Rodriguez has taken leadership of the Biorepository. All members of our team are passionate about improving the lives of women with pelvic floor disorders—and, through creative studies in the laboratory, working to prevent these conditions in the future!

Dr. David “Ike” Rahn has been the site PI for UT Southwestern since 2016. He graduated with a major in genetics from Texas A&M University. Ever since, he has been a proud UT Southwestern/ Parkland Hospital “lifer”, having completed his MD, Ob/Gyn residency, and fellowship training in Urogynecology at UTSW. PFDN participation has been foundational for Ike’s academic career. He especially values the collaborative and supportive interactions with researchers and mentors from PFDN sites across the country: “All our best work results from this multicenter team!”
Dr. Maria Florian-Rodriguez is an Assistant Professor in the Department of Obstetrics and Gynecology and a UT Southwestern Dedman Family Scholar in Clinical Care. She is a urogynecologist and specializes in the treatment of pelvic floor disorders. Maria earned her medical degree at the University of Puerto Rico School of Medicine. She completed a residency in obstetrics and gynecology at Temple University Hospital in Philadelphia and then received advanced training in urogynecology at UT Southwestern. She joined the UT Southwestern faculty in 2018. In the latest PFDN Cycle, she took over leadership of the UT Southwestern Biorepository, and she’s proud of the work of the PFDN Biospecimen Committee. She also chairs the Communications Committee.
Maria’s clinical interests include the surgical treatment of pelvic organ prolapse, urinary incontinence, mesh complications, and fistulas. Her research interests include studying the relationship between the vaginal extracellular matrix, cellular senescence, and prolapse.
A quote from Maria: “I’m passionate about treating women with pelvic floor disorders like urinary incontinence and pelvic organ prolapse because we have so many therapies that can dramatically improve their quality of life. These conditions are common – but it doesn’t mean women have to live with them!”


Agnes Burris, RN is our lead Clinical Research Coordinator for the PFDN, joining the Urogynecology division in taking on this role in 2018. Agnes spent many years as a critical care nurse in Parkland Hospital’s esteemed Burn Center/ ICU. In 1998, while still working in the Burn Center, she got her start in research nursing by organizing all the Center’s research data and coupled this with UT Southwestern’s burn research, caring for a premier database that has facilitated numerous publications and presentations.
If you speak with Agnes, you’ll recognize right away that her accent is not native to Texas! She hails from Greenock, Scotland. Agnes arrived in the US in 1982. She is passionate about family, horses, gardening, and woodworking, and she treasures spending time with her family and friends.
Helen Shi, Research Associate, has been an integral part of the PFDN Biorepository since its inception in 2010, when she worked alongside Dr. Ann Word (now retired) and Dr. Joseph Schaffer in the initial setup of the biorepository. She has been in charge of sample processing and analysis, as well as managing the database of sample storage for ABC, ROSETTA and RUM, NOTABLe, and PRoMISe studies. Currently, she works with Dr. Florian-Rodriguez on sample analysis of the PRoMISe study and sample collection for the upcoming TULIP-B study.

The University of Pennsylvania became a member of the Pelvic Floor Disorders Network (PFDN) in 2011, with Dr. Lily Arya serving as the site’s Principal Investigator (PI). Dr. Arya transitioned the role of PI to Dr. Heidi Harvie in 2021.
The Health System includes The Hospital of the University of Pennsylvania, the flagship hospital, Pennsylvania Hospital, Presbyterian Medical Center and several satellite Clinics, which allows us to draw a large and ethnically diverse patient population from the tri state area, Pennsylvania, New Jersey and Delaware.

Penn is at the forefront of Implementation Science, a relatively new field. Implementation Science lends tools to help reduce disparities and develop and scale effective innovations in healthcare. It recognizes the idea that there is a huge gap between the evidence that we produce in our standard research pathways and getting those evidence-based practices to the patients who need them. The PFDN has begun exploring opportunities to incorporate this new science into its research.

April 2024 Steering Committee Meeting Philadelphia: Dr. Lily A. Arya, Dr. Rebecca Hamm (Keynote Speaker, Implementation Science), Dr. Heidi S. Harvie, & Dr. Uduak U. Andy
Penn’s Urogynecology Research Team is comprised of 4 Urogynecologists, a Urologist, 3 Nurse Practitioners (Megan Carullo, Stephanie Haly, Diane Newman), 5 Research Coordinators (Zandra Kennedy (Project Manager), Shannah Ellis, Ngozi Ikpeama, Shyanne Hall and Alexis Singer). Shyanne and Alexis are the newest members of the team, both recent graduates of the University of Pennsylvania.
Although we may be a small team we have been described as “the little engine that could” with regard to our team’s contributions to Women’s Health Research.
Meet Our Physicians
Dr. Lily A. Arya, Chief, Division of Urogynecology and Pelvic Reconstructive Surgery, William Goodell, M.D. Professor of Obstetrics and Gynecology
Urogynecology as a specialty was “invented” just as Dr. Arya was completing her training. When she first met women with bladder issues and understood its impact on their lives, she knew this would be her chosen specialty. Dr. Arya has never looked back since. She was a Principal Investigator of the PFDN for 10 years and now serves as a co-investigator. What she enjoys most about the PFDN is talking with the patients who take part in our clinical trials. She is so impressed with their insightful questions and their desire to contribute to science. Many of their questions are helping us decide what studies to do and how to design these studies. Our patients’ participation is helping this generation of women and all the future generations to come.


Dr. Heidi S. Harvie, Director, Penn Urogynecology & Pelvic Reconstructive Surgery, Pennsylvania Hospital, Associate Professor of Obstetrics and Gynecology at the Pennsylvania Hospital
Dr. Harvie is the Principal Investigator at Penn for the current PFDN cycle and was previously the alternate PI. She has been involved in the PFDN since Penn became a site in 2011. What she finds so rewarding about being part of the PFDN is being able to work with such an amazing research team to design studies and conduct trials that make a difference in our patients lives. She is truly grateful for all the patients who choose to participate in our PFDN trials to improve the care for and the lives of other women. Dr. Harvie chose the field of Urogynecology because she loves helping the patient population of women with incontinence and prolapse improve their quality of life.
Dr. Uduak U. Andy, Chief of Gynecology at Penn Presbyterian Medical Center, Associate Professor of Obstetrics and Gynecology at the Hospital of the University of Pennsylvania
Dr. Uduak Andy is the alternate PI at Penn for the current PFDN cycle. She has been involved in the PFDN since she was a Urogyn fellow, and Penn became a PFDN site in 2011. She has had the privilege of working with and learning from some of the best and brightest research minds in pelvic floor disorders research. The most rewarding part of being a part of the PFDN is interacting with our amazing study participants. Dr. Andy is grateful for these women, many of whom participate in our trials to help answer some of the pressing questions in our field and ensure that we have the data to provide the best care for other women. She was drawn to the field of Urogynecology as it aligns with my personal life mission of helping women have the best quality of life possible. Conducting research through the PFDN ensures that she is doing that. As a mother of three young daughters, she is most proud that the research we conduct and the answers we discover may help provide the best care for future generations of women, including her girls!


Dr. Ariana L. Smith, Alan J. Wein II Professor of Urology, Chief of Urology Pennsylvania Hospital, Director of Urogynecology & Reconstructive Surgery, University of Pennsylvania Perelman School of Medicine
Dr. Ariana Smith is board certified in Urology and Female Pelvic Medicine and Reconstructive Surgery allowing her to care for women with a broad range of pelvic floor disorders and urinary complaints. Her research focuses on treatment of bothersome urinary symptoms and promotion of bladder health. The best part of her role in the PFDN is interacting with the amazing participants who volunteer for our studies. Dr. Smith’s patients have greatly enjoyed participating in the PFDN studies and take great pride in their contribution to science. She is incredibly proud of their unwavering dedication and selflessness in completing all their research visits. By sharing their time and experiences, they have contributed valuable insights that will significantly advance our understanding of pelvic floor disorders.
Recently Designated PFDN Coordinator
Shannah Ellis, Clinical Research Coordinator
Shannah Ellis joined the UPenn Urogynecology team in 2022, after graduating with a bachelor’s degree in Biobehavioral Health from Pennsylvania State University. During the past two years, she has been working with Dr. Uduak Andy on the “Move on Up Study,” an integrated exercise and bladder training intervention to reduce falls in older women with urinary incontinence. She looks forward to transitioning to working with the PFDN on the upcoming studies. Over the past couple of years, Shannah has had the opportunity to work closely with research participants, completing in-home visits, immersing herself within the community, and hearing first-hand about the obstacles that women with incontinence issues encounter. Her dedication to Urogynecology research stems from a desire to empower women with the knowledge of pelvic floor disorders, treatments, and potential prevention strategies. In her spare time, Shannah enjoys golf, reading, traveling, music, and spending time with friends and family. She is excited to contribute to the PFDN and making a lasting impact on women’s health outcomes!

In addition to taking part in Research and providing exceptional Clinical Care, the Team finds time to celebrate one another!

Celebrating Dr. Edward Kim on the completion of his Fellowship training in Urogynecology

Congratulations to Dr. Jaclyn Munoz on completion of her Fellowship in Urogynecology

Future Urogynecologist – we like to start training them young! (Dr. Munoz’s daughter, Zia)
RTI International is an independent nonprofit research institute dedicated to improving the human condition. RTI works in more than 75 countries and has offices on four continents, with headquarters in Research Triangle Park, North Carolina. RTI joined the PFDN as the data coordinating center (DCC) in 2011. The DCC works with the PFDN clinical sites to develop studies that help address critical issues in women’s urogynecological health. The DCC provides data collection tools and analyzes data from the studies so results can be published - ensuring the work done by the network reaches women with pelvic floor disorders and their providers.

Marie Gantz, PhD, Senior Fellow in Statistics, has served as the principal investigator of the PFDN data coordinating center since RTI was awarded the DCC in 2011. The DCC has worked with the clinical centers to launch nine clinical trials studying treatments for urinary incontinence, fecal incontinence, and pelvic organ prolapse. The treatments include pelvic floor muscle training, medications, devices, and surgeries. The results of these studies are published in medical journals, and for recent studies we have created videos that can be found on the website under Impactful Results.
Dr. Gantz has found it rewarding to be part of PFDN, because she gets to work with a great group of people – inside the DCC and across the network – to do meaningful research that helps women by finding better treatments for pelvic floor disorders.
Megan Carnes, PhD, serves as the Alternate Principal Investigator (PI). In this role she supports Dr. Gantz and the other team members in a variety of ways, especially with study design, biospecimen collection, and statistical analyses. Much of Dr. Carnes’s work focuses on translational and genomic studies. Translational research aims to bridge the gap between basic science and clinical practice. This is often done using genomics to study samples collected from urine, vaginal swabs, and the gut to look for biomarkers (a biological marker of a disease or response to treatment) of pelvic floor disorders.
Dr. Carnes finds the most rewarding part of the work on PFDN is the clinical impact. This means that the results of our research can make a difference in the lives of patients and their families, as well as the health care system.


Carolyn Huitema is the DCC Research Operations Manager and has been with the network since 2011, bringing extensive experience and dedication to her role. She collaborates with the clinical sites to implement meaningful clinical studies, by developing trainings, overseeing study operations, and helping to address challenges and establish best practices.
What Carolyn loves most about PFDN is the opportunity to collaborate with a network of passionate and dedicated researchers who share a common vision of advancing the science and practice of pelvic floor disorders. The PFDN’s research is not only exciting, but also meaningful and transformative for the lives of patients and providers.
Benjamin Carper serves as the DCC Statistical Operations Manager, specializing in harmonizing data monitoring and reporting for the network and coordinating the creation of public use datasets for completed PFDN studies. He also serves as a Senior Statistician developing and advising on the design and analysis of PFDN clinical trials. He has worked on the PFDN since 2015.
Ben loves knowing that the work of the PFDN is helping people improve their quality of life. Clean data, well-analyzed, can lead to valid and repeatable results that can influence medical practice. He also really loves working with such a diverse team of medical doctors and scientific professionals that show such dedication to helping people and wanting to move the field forward.


Tucker Brenizer leads the development of the PFDN research systems and helps improve operations using data insights. More specifically, Tucker works with a group of programmers, analysts, and data managers to find the most efficient and cost-effective ways to meet the PFDN’s systems and data management needs. The key to success in this goal is the regular feedback that is received from the PFDN coordinators and collaborators, for whom he is sincerely grateful
Tucker has been with the PFDN since 2021. He has genuinely enjoyed learning from the other members of the RTI Team and getting to know our many site collaborators.
Meet Kyle Herrala, MS, Clinical Research Project Manager at UCSD!

This month we recognize Kyle Herrala, MS, Clinical Research Project Manager for the Division of Urogynecology and Reconstructive Pelvic Surgery at UCSD. She also serves as the chair of the PFDN Research Coordinator Committee. She has been with the PFDN for almost 7 years and oversees all active research studies as well as manages the single-IRB for all participating sites in the PFDN.
Ms. Herrala was recently honored as the 2024 recipient of the Robin Haff Research Award at the American Urogynecologic Society (AUGS) conference held in Washington, DC in October. We congratulate her for her achievements!
Ms. Herrala began her career working in community health. She has always been passionate about health education and disease prevention and is a firm believer that quality health starts with the simple choices we make at home. Her interest in health prevention led her to earn a Master of Science in Health Education and Health Behavior. She worked with various non-profit organizations in areas such as food insecurity, childhood health and fitness, sexual assault and domestic violence prevention, and mental health. Ms. Herrala began working at UCSD and with the PFDN in 2018. The most rewarding part of working with the PFDN is being able to connect with patients and see first-hand the real-world impact of the work we are doing. She also loves being a part of the bigger picture goal to improve healthcare for women and having been with the network for so long now, has enjoyed seeing the how our research has directly affected patient care.


Ms. Herrala grew up in the Midwest and went to the University of Michigan (Go Blue!). She’s lived in San Diego for almost 10 years and absolutely loves it there! She can always be found outdoors either at the beach, camping in the mountains, or hiking with her husband and two kids. A few years ago, she set out to hike 52 trails in one calendar year, hiked the highest 6 peaks in Southern California, and summitted Mt. Whitney (the tallest peak in the contiguous US). She also enjoys yoga and is a certified instructor. Her favorite thing is sharing all of these adventures with her family.

Deborah L Myers MD
Dr. Myers has been in the subspecialty field of treating women with pelvic floor disorders for over 30 years. Her career as Division Director entailed building the Urogynecology Division at Women and Infants Hospital of RI/ Brown to ensure that the diagnosis and treatment of pelvic floor disorders was of wide range for the women of southern New England, along with building strength in research and education. Her administrative role as Vice Chair of the Department of OBGYN also helped to strengthen the research mission at the institutional level. Dr. Myers first became affiliated with the Eunice Kennedy Shriver National Institute of Child Health and Human Development Pelvic Floor Disorders Network as a member of their Advisory Board (2007- 2010). In this role she had the opportunity to guide network researchers in their queries and see how high-level multi-site trials were conducted. This role allowed her to incorporate ideas into the Brown division to further build their research infrastructure. This led to Brown’s successful application as a site for the PFDN in 2011 cycle #3 (2011-2016) where she served as Principal Investigator from 2011-2014. Brown has continued participation in the network for cycle 4 (2016-2022) and the current #5 cycle (2022-2027). As a PFDN site, Brown offers a high volume with multi-disciplinary and translational collaborators.
What is unique about PFDN research?
The PFDN has been a highly active network since its start in 2001 performing research trials to answer key clinical questions for women with pelvic floor disorders. In general, there are 5-7 trials at any one time either in development, active, or analyzing data of completed trials. Over 150 studies have been published in high tiered journals including landmark trials in Journal of the American Medical Association (JAMA) and the New England Journal of Medicine (NEJM) which shows the high caliber research being done in the PFDN. Notwithstanding the network’s high productivity, Dr. Myers finds the most unique aspect of PFDN research is its success in developing and executing surgical trials. Simply said, these are research trials that look at whether one surgical procedure is more successful than another and/ or if concomitant procedures/treatments are beneficial or not. Surgical trials are quite difficult to develop and execute, i.e., recruit for, as they need to ensure equipoise for the patient, relevancy, and the support and commitment of all the investigators in the network.

Deb Myers retirement group photo at the July 2024 Steering Committee meeting

AUGS, August 2018: Vivian Sung MD MPH (co-PI 2011-2014 and PI 2014- current), Charles Rardin MD (co-PI 2024-current), Deb Myers (PI 2011-2014 and co-PI 2014-2024)
What do you consider your most significant contribution to the PFDN?
Dr. Myers considers her most significant contribution to the PFDN when serving as chair of the Policy Procedures Quality Improvement (PPQI) Committee from 2011-2015. During this time, she drafted the PPQI manual which involved documenting the processes and roles of the steering committee, its officers, the Data Safety and Monitoring Board, the Advisory Board and its outside collaborations. The manual also created committee descriptions, voting actions, policies and protocols by which manuscripts and abstracts are processed, and several other aspects of PFDN work. Dr. Myers worked with Susie Meikle, MD, MPH who was the project scientist of the PFDN at that time. The manual took about 4 years to complete as it involved input and consensus from all Principal Investigators of the PFDN. She often referred to it as “herding cats” (LOL). The PPQI manual has since served as a base for updating policies and creating new ones, as it is truly a “living document”. Her most recent contribution to the PFDN was serving as chair of the pelvic organ prolapse quantification (POP-Q) adjudication committee and later assessing and drafting as writing team chair a manuscript that describes the network’s quality metric tools to improve data quality for POP-Q data.
What impact have you seen over the time you’ve been involved with the PFDN?
Besides the high-quality research done to answer clinical questions, Dr. Myers believes the PFDN through its research has been able to raise awareness of the condition of pelvic floor disorders to both patients and other medical professionals. Awareness to patients has increased from the studies done; the outreach to women that is needed to perform these trials increases the public’s knowledge about PFDs. Awareness of PFDs to medical professionals outside of gynecology has happened through the network’s s publications in non- OBGYN journals such as JAMA and NEJM. More health care professionals are asking patients about pelvic floor disorders and referring them to subspecialists.

2011 Vivian Sung MD MPH, Deb Myers MD

April 2015- Myers awarded the “PPQI” prize at the PFDN SC meeting Rockville MD
What do you envision for the PFDN in the next 10 years?
Through the PFDN’s continued research efforts and intent on including populations of a more diverse background, Dr. Myers predicts there will be increased inclusion of underrepresented patients. This in turn will increase awareness and education of PFDs amongst these diverse women and thus improve health care of all women. Another aspect she hopes to see for the PFDN is an increase in the basic science research of PFDs. As the subspecialty and its basic science research continues to grow, she awaits more research into the pathophysiology of PFDs, the ability to identify women at risk for PFDs and the science to regenerate tissues in pelvic floor disorders. Dr. Myers anticipates regenerative medicine will be a big part of health care in the future and looks forward to more basic science into PDFN research which will move the field forward over the next years.
What has been the most rewarding part of working with PFDN?
For Dr. Myers, besides being part of a network which has led to answers for significant clinical questions in the treatment and management of PFDs, the most rewarding aspect of working within the PFDN has been the ability to collaborate with researchers across the country. The exchange of ideas is open and honest and always leads to a better trial. The relationships that have developed amongst all the staff, which is the staff of the PFDN, the data coordinating center, the other site’s researchers and their staff, have been incredible and the most fulfilling. It has been an honor for her to work with this high level of group of researchers.

July 2015 PFDN Duke SC meeting- Vivian Sung MD MPH and Deb Myers MD with Wool E. Bull